Abstract
INTRODUCTION: Hematopoietic stem cell (HSC) transplantation and ex vivo HSC gene editing are curative treatments for Sickle cell disease (SCD). Both, however, require myeloablative conditioning with its associated risks. In utero hematopoietic cell transplantation offers a potential non-myeloablative alternative but is limited clinically due to the acquisition of T cell immunity in the human fetus in mid-gestation and the technical and practical challenges of early-gestation transplantation. We have previously demonstrated that transient T cell depletion with anti-CD3 monoclonal antibody (mAb) restores allograft receptivity in a non-diseased mouse model of late-gestation allogeneic transplantation. Here we investigate whether late-gestation allogeneic transplantation with transient T cell depletion can successfully treat SCD in the Townes mouse model.
METHODS: Townes mice are mixed B6 background (H2kb) mice in which the endogenous murine beta globin genes have been replaced by human hemoglobin knock-in genes. Twenty-million T cell-depleted (TCD) Balb/c (H2kd) bone marrow cells (BMCs) were transplanted along with 5mg/kg of anti-CD3 mAb into homozygous (ßS/ßS) Townes mice shortly after birth at 20.5 days post-coitum (DPC) via the facial vein. Mice were analyzed at 1, 2, 3, 4, 8, 12, and 16 weeks of age for T cell recovery and donor leukocyte engraftment by flow cytometry, anemia by complete blood count (CBC), and the relative prevalence of murine (donor-derived) and human (host-derived) hemoglobin by high performance liquid chromatography (HPLC). Terminal analysis was performed at 16 weeks of life including: hypoxia-reoxygenation (10% O2, 6 hours; 21% O2, 16 hours) with subsequent in vivo and ex vivo sickling assays as well as assessment of hepatosplenomegaly and bone marrow lineage-c-kit+sca-1+ (LSK) donor engraftment. Uninjected, age-matched homozygous (ßS/ßS) and heterozygous (ßA/ßS) mice served as diseased and healthy controls.
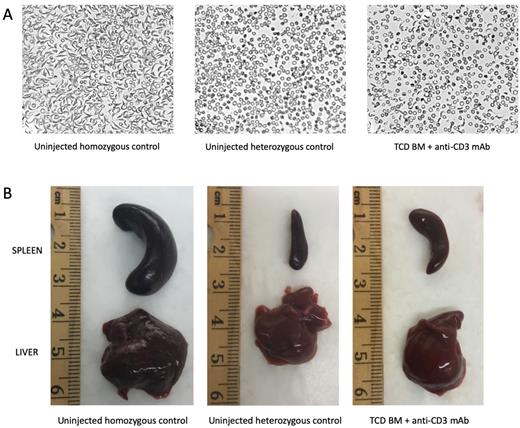
RESULTS: Long-term donor cell engraftment was achieved (mean peripheral blood leukocyte chimerism: 2.1 ± 1.6%; mean bone marrow LSK chimerism: 0.9 ± 1.0%) with donor-derived reconstitution of all hematopoietic lineages, including T cells, B cells, monocytes, and granulocytes. Recipient T cells recovered from antibody-mediated depletion to normal levels at 3 weeks of age. Significant improvement in anemia by CBC was sustained to the study endpoint (9.7g/dL among transplanted mice vs. 7.5g/dL among uninjected homozygous controls (P<0.001) vs. 12.2g/dL among uninjected heterozygous controls (P<0.001)). The mean percentage of murine (donor-derived) hemoglobin by HPLC was 35.6 ± 21.2% at terminal analysis, demonstrating the survival advantage of donor-derived (non-sickled) erythrocytes compared to host-derived (sickled) erythrocytes. Ex vivo sickling assay showed a significant decrease in sickled cells compared to uninjected homozygous controls (mean: 40.7 ± 7.7% vs. >90% among uninjected homozygous controls (P = 0.001) vs. 0% among uninjected heterozygous controls (P < 0.001); Figure 1A) with associated improvement in hepatosplenomegaly (Figure 1B). In vivo sickling following hypoxia was similarly decreased among transplanted mice (mean: 28.6 ± 10.5%). Transplant recipients gained weight normally with no signs of graft-versus-host disease.
CONCLUSION: Late-gestation allogeneic transplantation with transient T cell depletion results in long-term donor cell engraftment with significant improvement of the disease phenotype in the Townes mouse model of SCD. This approach may be a useful strategy by which to achieve clinical cure of SCD without myeloablation and its associated risks.
Disclosures
Dave:Vitara Biomedical: Ended employment in the past 24 months.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal